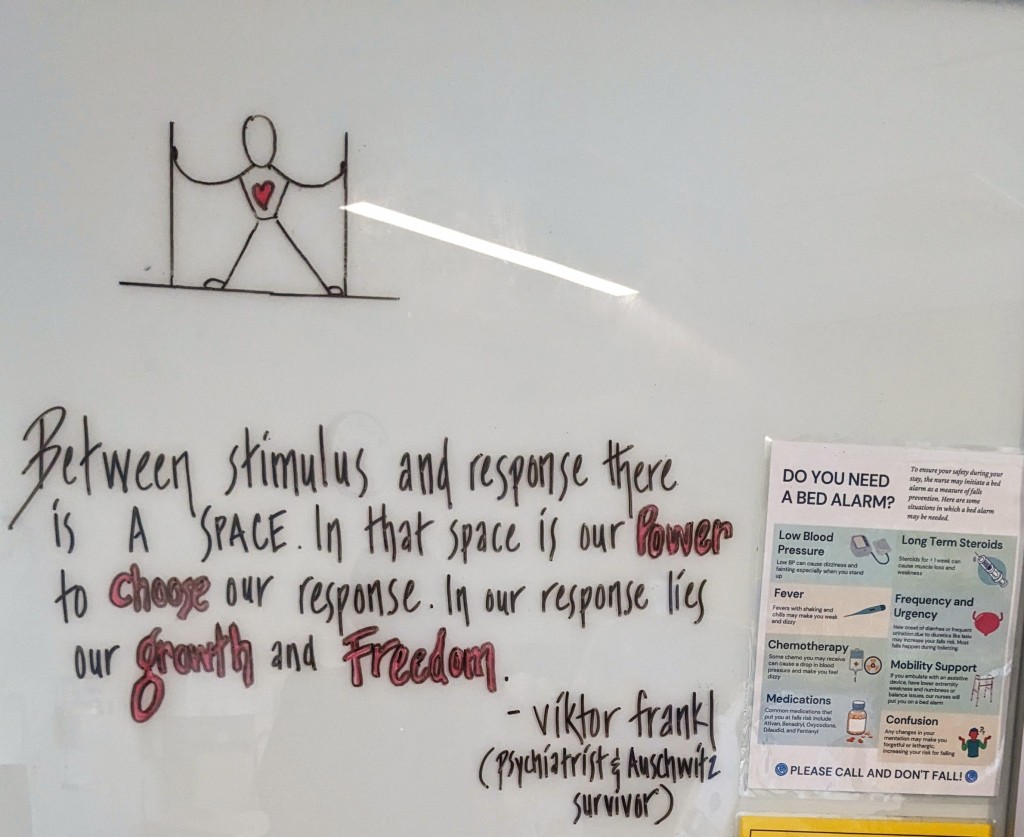
One of the quotes we put up on the whiteboard of Viral’s hospital room
This is not a journey for the faint of heart. A CT scan a few days ago reveals a lesion in Viral’s right lung, indicative of a fungal infection. This, in addition to the bacterial infection already in his system. In order to get a clearer picture of what is going on, a series of blood cultures, chest x-rays, CT scans, an ultrasound, and echocardiogram are ordered. Infectious disease specialists are brought in to determine the best course of action. In an attempt to provide broader, stronger coverage, a new set of powerful antibiotics and anti-fungal medications are added to his regimen. Extra fluids are pumped into his body to protect his kidneys from side effects of the new drugs. This, at a time when he is still struggling with fluid retention, and still on a daily dose of diuretics. Additional complications from GI tract issues and related pain play havoc with his system. His temperature rises, his oxygen levels fall and his pulse rate soars. Two nights ago, as all of these various forces converge, his heart, his strong, steady heart, is thrown dizzyingly out of rhythm. The nurses leap into action. Within minutes they have him on an EKG, and a doctor is in the room, reading the charts and figuring out the best course of action. In this case a low dose beta blocker by IV to bring his heart rate down and resettle his system.
In the early hours of the morning his heart rate escalates wildly again. Even slight exertion now triggers acute dysregulation. Simultaneously and related to all of this, fluid is continuing to build up internally with no way of releasing on its own. A rapid response team rushes in. Medication is swiftly administered and a special catheter inserted to allow his system to discharge fluids more easily. Adjustments and further adjustments are made to his pain medications. A decision is made to pull out his central line — a possible source or repository for infection. A double dose of platelets are transfused in advance, and IV lines inserted peripherally in his veins so that he can continue receiving the multiple streams of medications needed in this time. “We’ve got you,” the nurses, the phenomenal nurses say this to us, over and over again. Sometimes there are more than half a dozen of them in the room with us, covering for all possibilities, meeting the exigencies of the moment with confident competence, and such compassion.
***
To successfully subdue the presence and growing threat of infections it is vital for Viral’s immune system to come online. Neutrophils– a particular kind of white blood cell– are the most powerful anti-bacterial and anti-fungal agents we have. But at this juncture engraftment has yet to take place. It is +18 days since transplant. The old immune system has been effectively shut down and the new one has not yet set up shop. For weeks now his WBC count has been less than 0.1 In this vacuum his susceptibility to further infections is high. The toll on his body is intensified. Sitting with him, not long after we had learned of the presence of a bacterial infection in his blood, I ask Viral a few questions…
How are you holding this new piece of information?
One– you gotta roll with whatever is happening. And two– we’re still not even close to pushing what the edges of the medical system can and has handled. Sure the risks go up with each of these things but there are still a lot of tools at their disposal. [Too much realism and you’re in danger of being a cynic, too much trust and you’re in danger of being naive. How I love him. This being whose way lies in the sweet spot between the two. It’s what enables him to engage head on with reality without ever losing the spirit of possibility.]
Can you describe some of what you’re experiencing at a physical level?
Obviously different kinds of discomforts. A lot of it is focused around the hemorrhoid pain. There is something about the constancy of the discomfort that becomes its own challenge — different from the acute episodic aspect that is also present. So I am navigating both of those things. And then there’s the extreme bodily weakness and fatigue, the fevers, the drowsiness, the brain fog, canker sores, the challenges with retaining fluids, the erratic heart rate, low oxygenation and all the rest of it. Somehow the main asset in all of this has been kind of really remaining present to the present experience. It’s not even a conscious attempt at doing this, it just happens.
There are so many harsh changes taking place in the body as a result of all these side effects — the dark patches on the skin, itchy palms and feet, dry mouth and chapped lips, the considerable swelling of feet and legs, the tremors, the inability to lie flat without coughing, the blood in your phlegm. The difficulty in doing things that used to be simple — standing up, walking, eating, using the restroom. How do you experience all of this change without being dampened by it?
We know that biologically, with all the medications and chemo, and now these infections, I’m in sort of really slowed down microbiome state, and that has all these implications on the neurotransmitters [that give us a sense of well-being, motivation and general positivity]. So there’s the layer at which all those things are sense-able, in that I can sense that suppression. But it doesn’t generate strong identification. In a way it can just be revealing. It’s not like pain has no effect on me or anything like that. It’s clearly unpleasant. But it’s not creating these energetic flows of harping on the unpleasantness, it doesn’t spin off into projecting this pain into the future. It’s like, “Yes the unpleasantness is here, now.” And the story kind of ends there. [To witness him interfacing in such a quiet, understated and humble way with the many bodily hardships, the chaotic episodes and dramatic alterations of this time, breaks my heart and simultaneously swells it with love and amazement. I am awed all over again by the gift of this being, and the gift of being by his side.]
There is a change in your expression and body language when you have been navigating pain over a long period. Your usual sunniness and availability is dampened, and from the outside it could seem like you are really down. But knowing you, I know it’s not quite that. How would you describe it?
There is a transparency to all this. There is definitely something happening, and that shows up in my expression and posture. In those moments I think what my body is reflecting is an engagement with the unpleasantness. But my experience of that engagement is not a feeling of down-ness. Right now there is just not the same kind of residue that I myself have experienced in the past with pain. Maybe there’s just not as much resistance. Shinzen Young has a neat equation for this: Suffering = Pain x Resistance. So yes there’s pain that I am feeling, but there’s not a lot of suffering because there’s not a lot of resistance.
***
I am so grateful to be able to spend almost all of each day, and every other night, here with him at the hospital. Nipun alternates nights with me, and Guri is here for a good part of each day as well, while also constantly planning for and making meals to nourish our journeys. Both of them are unconditionally making so much possible for both of us. (And many others are holding all of us through this time in visible and invisible ways.) Between us we are able to ensure that one or more of us is with Viral at all times. In the wee hours of last night, as he drifts in and out of sleep with so many different wires and tubes tethering his tired body, I lean over and placed my palm in one of his. His fingers curl over mine. I feel the warm clasp of his hand, as familiar to me as my own. A small squeeze, a caress from his thumb. Even half asleep and wracked by many ills, he is sending some of his strength and love, my way. May I receive both as deeply as I can.
***
It is the evening of Day 19. He is more stable now on certain fronts, but has been more fatigued than usual today, and he is starting a fever (again). His head hurts and he has not had the energy to speak much, but he makes an effort to ask the night nurse about his labs. She writes them on the whiteboard on the wall across from his bed. Platelets 65k (thanks to a transfusion this morning of two units). Hemoglobin 7.2 (holding steady from yesterday, so no RBC transfusion tonight, but likely one tomorrow). And WBC 0.1.
0.1. It takes a moment to register this information. A number so small it seems negligible. But it’s not. It’s a detectable amount. It’s something after a long time of nothing. It is too early to say for certain, there is still much to be resolved, and it could still take a while. It could still dip into nothingness again. A sign so small it almost feels silly to take it seriously. But this is how it starts we’ve been told. Engraftment. A glimmer, a glint. A little flash on the horizon. Viral smiles faintly.
I think of something N, the nursing assistant with a flower-bright face and a lovely simplicity of heart, shared not long ago when I asked her if there was a quote or any words of wisdom that particularly resonated with her. “Oh! Let me think,” she said. And then after a few moments of pause–
“Anything’s Possible.”
0.1.
Anything’s possible.

